What is Irritable Bowel Syndrome (IBS)?
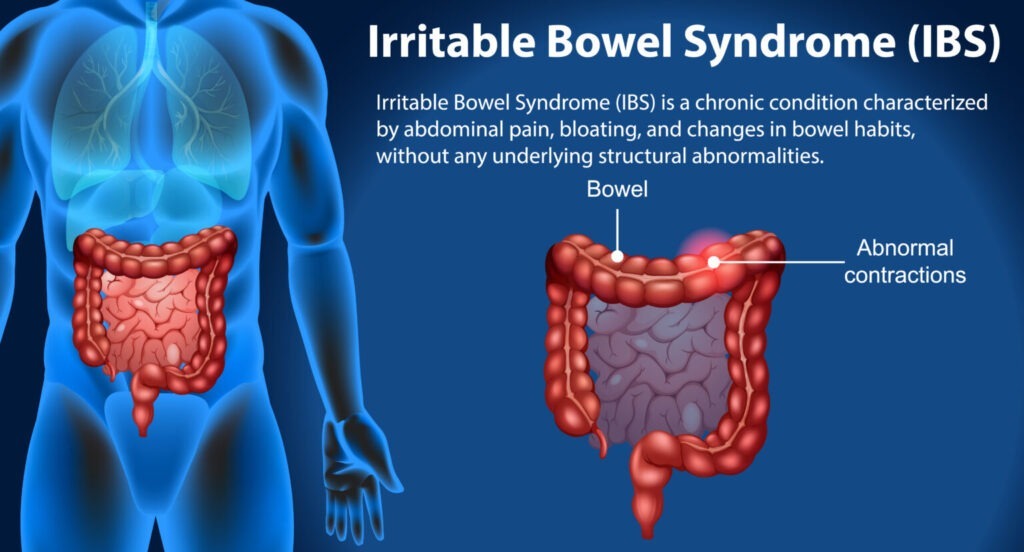
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder characterized by a combination of symptoms affecting the large intestine. While the exact cause of IBS remains unclear, it is believed to involve a complex interplay of factors including abnormal intestinal motility, visceral hypersensitivity, alterations in gut microbiota, inflammation, and psychosocial factors.
Symptoms of IBS can vary widely among individuals and may include abdominal pain or discomfort, bloating, changes in bowel habits (such as diarrhea, constipation, or alternating between the two), excessive gas, urgency, and a feeling of incomplete bowel movements. These symptoms can significantly impact an individual’s quality of life, leading to missed workdays, social isolation, and psychological distress.
It is important to distinguish between IBS and other gastrointestinal disorders such as inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis. Unlike IBD, which involves inflammation and structural damage to the digestive tract, IBS is considered a functional disorder, meaning there are no visible signs of disease on diagnostic tests like colonoscopy or imaging studies.
Types and Subtypes of Irritable Bowel Syndrome
IBS can manifest in various forms, which are primarily categorized based on stool consistency during symptom flare-ups. These include:
- IBS with Constipation (IBS-C): Characterized by infrequent bowel movements and hard, lumpy stools.
- IBS with Diarrhea (IBS-D): Characterized by frequent, loose or watery stools.
- IBS with Mixed Bowel Habits (IBS-M): Characterized by alternating periods of constipation and diarrhea.
- Unclassified IBS (IBS-U): When symptoms do not fit into the above categories or when individuals experience a combination of symptoms from different subtypes.
Understanding the different types and subtypes of IBS is important for tailoring treatment approaches to individual needs and preferences.
Prevalence and Impact of Irritable Bowel Syndrome (IBS)
IBS is one of the most common gastrointestinal disorders worldwide, affecting approximately 10% to 15% of adults. However, due to underreporting and misdiagnosis, the true prevalence may be even higher. IBS is more common in women than men, and symptoms often begin in early adulthood.
The impact of IBS on an individual’s quality of life can be significant. In addition to physical symptoms, IBS can lead to emotional distress, anxiety, and depression. It can also interfere with social activities, work, and relationships, leading to decreased productivity and increased healthcare utilization.
Causes and Triggers of IBS
The exact cause of IBS remains unclear, but it is believed to involve a complex interplay of factors. These may include:
- Abnormal intestinal motility: Dysfunction in the coordination of muscle contractions in the intestines can lead to symptoms such as diarrhea, constipation, or abdominal pain.
- Visceral hypersensitivity: Increased sensitivity to pain signals from the gut can result in heightened perception of discomfort or pain.
- Alterations in gut microbiota: Imbalances in the composition of gut bacteria (dysbiosis) may contribute to symptoms of IBS.
- Inflammation: Low-grade inflammation in the gut may play a role in some cases of IBS.
- Psychosocial factors: Stress, anxiety, depression, and other psychological factors can exacerbate symptoms of IBS.
- Genetic predisposition: Family history of IBS or related conditions may increase the risk of developing the disorder.
- Environmental factors: Diet, lifestyle, and environmental triggers such as infections or food intolerances may contribute to symptom onset or exacerbation.
Identifying triggers, such as certain foods, stressors, or hormonal changes, is essential for managing IBS symptoms effectively.
Symptoms and Clinical Presentation
Symptoms of IBS can vary widely among individuals and may include:
- Abdominal pain or discomfort: Typically located in the lower abdomen and often relieved by bowel movements.
- Bloating and distention: A sensation of fullness or swelling in the abdomen, often accompanied by visible swelling.
- Changes in bowel habits: These may include diarrhea (frequent, loose stools), constipation (infrequent or difficult bowel movements), or alternating between the two.
- Excessive gas (flatulence): Increased production of gas in the intestines, leading to bloating and discomfort.
- Urgency: A sudden, intense need to have a bowel movement.
- Feeling of incomplete evacuation: The sensation that bowel movements are not fully emptied, even after passing stool.
- Mucus in the stool: The presence of mucus (a clear, jelly-like substance) in the stool, which may indicate inflammation or irritation of the intestines.
These symptoms can occur either persistently or during intermittent flare-ups, and their severity can vary over time.
Diagnosis of Irritable Bowel Syndrome
Diagnosing IBS involves a comprehensive evaluation by healthcare providers, often based on symptom criteria such as the Rome criteria. Diagnostic tests may include:
- Medical history: Detailed questioning about symptoms, triggers, and medical history.
- Physical examination: Examination of the abdomen for tenderness, distention, or masses.
- Blood tests: To rule out other conditions such as celiac disease, thyroid disorders, or inflammatory markers.
- Stool studies: To check for infections, parasites, or malabsorption.
- Imaging tests: Such as colonoscopy or sigmoidoscopy to visualize the colon and rule out structural abnormalities or other gastrointestinal disorders.
A diagnosis of IBS is typically made after other gastrointestinal conditions have been excluded. It is important for individuals to communicate openly with their healthcare providers about their symptoms and concerns to ensure an accurate diagnosis and appropriate management plan.
Treatment Options for Irritable Bowel Syndrome (IBS)
Treatment strategies for IBS focus on alleviating symptoms and improving quality of life. These may include:
- Lifestyle modifications: Dietary changes (e.g., low-FODMAP diet), regular exercise, stress management techniques (e.g., relaxation exercises, mindfulness meditation).
- Medications: Antispasmodics (e.g., dicyclomine, hyoscyamine), laxatives (e.g., polyethylene glycol, lubiprostone), probiotics, antidepressants (e.g., tricyclic antidepressants, selective serotonin reuptake inhibitors), and newer agents like alosetron and eluxadoline.
- Behavioral therapy: Cognitive-behavioral therapy (CBT), gut-directed hypnotherapy, biofeedback.
- Alternative therapies: Acupuncture, herbal supplements (e.g., peppermint oil), yoga, and mindfulness meditation.
Individualized treatment plans are tailored based on symptom severity, subtype of IBS, and patient preferences. It may require a trial-and-error approach to find the most effective combination of treatments for each individual.
Prognosis and Outlook
Living with IBS requires long-term management, but most individuals can effectively control their symptoms with the right treatment plan. While there is no cure for IBS, proactive management strategies and ongoing research offer hope for improved outcomes and enhanced quality of life.
With proper treatment and self-care measures, many people with IBS are able to lead fulfilling lives and maintain normal daily activities. It is important for individuals to work closely with their healthcare providers to monitor their symptoms, adjust their treatment plan as needed, and address any concerns or challenges that may arise.
While IBS can be challenging to live with, it is important to remember that there is support available and that you are not alone in your journey. By staying informed, seeking support from healthcare professionals, and exploring personalized treatment options, individuals with IBS can effectively manage their symptoms and improve their overall well-being.
Future Directions in IBS Research
Ongoing research in the field of IBS aims to uncover novel treatments and therapies that may provide additional options for symptom relief and management. Some areas of interest include:
- Fecal microbiota transplantation (FMT): Transplanting healthy gut bacteria from a donor into the intestines of individuals with IBS may help restore microbial balance and improve symptoms.
- Targeted pharmacotherapies: Developing medications that target specific pathways involved in the pathophysiology of IBS, such as serotonin receptors or gut motility.
- Biomarkers: Identifying biomarkers in blood, stool, or other biological samples that can aid in the diagnosis and monitoring of IBS.
- Neurogastroenterology: Advancements in understanding the complex interactions between the gut and the brain may lead to new insights into the underlying mechanisms of IBS and novel treatment approaches.
- Personalized medicine: Tailoring treatment approaches based on individual characteristics such as genetics, microbiome composition, and symptom profiles.
Clinical trials exploring these and other emerging therapies hold promise for enhancing symptom control and addressing the underlying causes of IBS. It is important for individuals with IBS to stay informed about ongoing research and discuss potential treatment options with their healthcare providers.
Conclusion
In conclusion, Irritable Bowel Syndrome is a complex gastrointestinal disorder with diverse manifestations and treatment challenges. By understanding its underlying mechanisms, identifying triggers, and adopting a holistic approach to management, individuals with IBS can regain control over their lives and experience symptom relief.
It is important for individuals with IBS to stay informed about their condition, communicate openly with their healthcare providers, and explore personalized treatment options. With proper management and support, many people with IBS are able to lead fulfilling lives and maintain their overall well-being.
Remember, you are not alone in your journey with IBS. There is hope for symptom relief and improved quality of life, and by staying proactive and engaged in your care, you can effectively manage your symptoms and thrive.
Frequently Asked Questions about Irritable Bowel Syndrome (IBS)
1. Is IBS a serious condition?
- Many people wonder about the severity of IBS and whether it poses significant health risks.
2. Can stress worsen IBS symptoms?
- Stress is often linked to digestive issues, but its specific impact on IBS symptoms is a common concern.
3. Are there specific foods that trigger IBS symptoms?
- Individuals often seek information on dietary triggers and foods to avoid to manage their IBS symptoms better.
4. What role does gut health play in IBS?
- People are increasingly interested in understanding the connection between gut health, gut microbiota, and the development of IBS.
5. Are there natural remedies or home treatments for IBS?
- Many individuals explore alternative therapies and home remedies to alleviate their IBS symptoms, seeking information on their effectiveness.
6. Can IBS affect mental health?
- The relationship between IBS and mental health conditions like anxiety and depression is a common topic of inquiry.
7. How does IBS impact daily life and activities?
- Individuals often inquire about the practical implications of living with IBS, including its effects on work, social activities, and travel.
8. Can IBS symptoms change over time?
- People may wonder whether IBS symptoms remain constant or if they fluctuate or evolve over time.
9. Is there a link between IBS and other medical conditions?
- Many individuals seek information on potential comorbidities or connections between IBS and other health issues.
10. Can IBS be managed without medication?
- Some individuals prefer non-pharmacological approaches to managing their IBS symptoms and seek guidance on alternative treatment options.
5 Tips to Tame Gut Inflammation & Boost Health
